Regular Pulse
Your pulse is your heart rate, or the number of times your heart beats in one minute. Pulse rates vary from person to person. Your pulse is lower when you are at rest and increases when you exercise (more oxygen-rich blood is needed by the body when you exercise). Knowing how to take your pulse can help you evaluate your exercise program.
Part II: Assessment Techniques
Inspection
As you prepare to begin the actual assessment, you already have obtained and recorded the patient history and you arm yourself with pertinent data such as their chief complaint and allergic history.
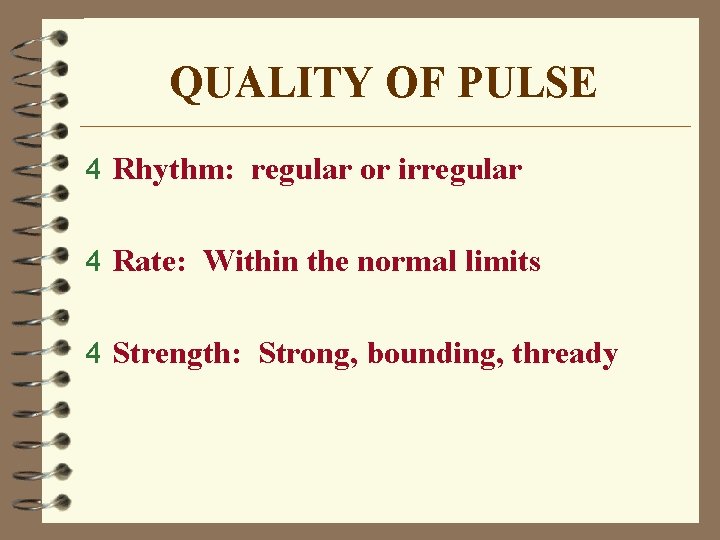
- The normal pulse rhythm is regular, meaning that the frequency of the pulsation felt by your fingers follows an even tempo with equal intervals between pulsations. If you compare this to music, it involves a constant beat that does not speed up or slow down, but stays at the same tempo. Thus, the interval between pulsations is the same.
- A hare-brained idea, in my opinion, as even a regular pulse can be hard to feel and an irregular one can even present problems for a qualified doctor. New heart research may prevent stroke The scientists then implanted pressure sensors and artificial hearts, small bulbs pumped with fluid that produce the illusion of a regular pulse.
- A normal resting heart rate for adults ranges from 60 to 100 beats per minute. Generally, a lower heart rate at rest implies more efficient heart function and better cardiovascular fitness. For example, a well-trained athlete might have a normal resting heart rate closer to 40 beats per minute. To measure your heart rate, simply check your pulse.
- The normal pulse for healthy adults ranges from 60 to 100 beats per minute. The pulse rate may fluctuate and increase with exercise, illness, injury, and emotions. Females ages 12 and older, in general, tend to have faster heart rates than do males. Athletes, such as runners, who do a lot of cardiovascular conditioning, may have heart rates.
Also keep in mind to allow a certain amount of time in order to complete a thorough exam. Many nurses do not have large blocks of time for completion of the assessment but you must be as thorough as possible. If this is an admission assessment, you must allow enough time to be complete. If this is an on-going assessment, not as much time will be required.
Begin Exam
- Patient undresses, but allow for privacy.
- Have the patient sit upright and inspect the thorax from the front.
- Now inspect from the back of the patient.
You will inspect for posture and symmetry of the thorax, color of the skin, gross deformities of the skin or bone structure, the neck, face, eyes, and any abnormal contours. Breathing patters will also be noted. Be especially aware of the presence of cyanosis. Central cyanosis is a condition which will cause the lips, mouth, and conjunctiva to become blue. Peripheral cyanosis will cause blue discoloration mainly on the lips, ear lobes, and nail beds. Peripheral cyanosis might indicate a peripheral problem of vasoconstriction, and would generally be less severe than central cyanosis, which could indicate heart disease and poor oxygenation.
Thorax
Inspect for symmetry of thorax, point of maximum intensity (PMI). PMI is easier to find if the patient will lay on the left side. PMI may also be palpated. Check skin color of thorax.

Eyes
Arcus Senilis is a light gray ring surrounding the iris, common in older patients; in younger patients it might indicate a type of lipid metabolism disorder, which is a precursor to coronary artery disease.
Xanthelasma is yellowish raised plaques on the skin surrounding the eyes. Can also appear on the elbows. This is a possible indication, or sign of hypercholesterolemia, often a precursor to coronary artery disease (atherosclerosis).
Palpation

Palpation, or touching, is the next part of the exam. In the stop above, if we noted any abnormalities, we will now palpate and evaluate them further.
Skin: temperature, texture, moisture, lumps, bumps, tenderness.
Examination of extremities for edema might also indicate a cardiovascular problem. Examine the feet, ankles, sacrum, abdomen, trunk, and face for edema. If you notice puffiness of frank edema, then palpate the area for pitting edema. Most facilities recognize the following scale:
+1 Pitting Edema | = | 0 to ¼ inch indentation |
+2 Pitting Edema | = | ¼ to ½ inch indentation |
+3 Pitting Edema | = | ½ to 1 inch indentation |
+4 Pitting Edema | = | More than 1 inch indentation |
Breathing: lay hands the chest at different locations and feel the respiratory patterns, feel the ribs elevate and separate during normal breathing.
Pre-Cordial Areas you can feel the pounding of the heartbeat, normal and abnormal pulsations o the chest wall; PMI, as mentioned above.
Arteries: Assess all pulses
Regular Pulse Range
You undoubtedly assessed the apical pulse earlier when you took the patient’s vital signs, if not, now is the time. Assess the following pulses:
Regular Pulse Reading
- Apical heart rate – monitor for a full minute, note rhythm, rate, regularity.
- Radial pulse – monitor for a full minute. Note the rhythm, rate, and the regularity. Note any differences from right to left radial, a large difference might indicate arterial blockage or even enlarged ventricles. If pulse is regular but volume diminishes from beat to beat, this might indicate left-sided heart failure and is called pulses alternans. If the volume of the pulse diminishes on inspiration, might indicate constrictive pericardial disease, the condition is called pulsus paradoxus.
- Carotid, brachial, femoral, popliteal, posterior tibialis, and dorsalis pedis pulses – when checking these pulses do it the same way as the others mentioned in this section; right then left side. When you check the carotid, press gently and do not rub.
Do not palpate carotid on persons with known carotid disease or bruits; listen with stethoscope instead; and do not palpate both carotid pulses at the same time.
Carotid Artery:
- Plateau pulse – slow rise and slow collapse pulse; may be caused by aortic stenosis, slow ejection of blood through a narrowed aortic valve.
- Decreases amplitude (grade point pulse) – due to hemorrhagic shock, pulse is weak due to decreased blood volume.
Heart Rate Chart
Bounding Pulse - (Grade IV) can be due to hypertension, thyrotoxicosis, others; associated with high pulse pressure, the upstroke and downstroke of the pulse waves are very sharp.
Regular Pulse Reading
It is common to use +1, +2, etc. when recording pulses:
- 0 = absent
- +1 = diminished or decreased
- +2 = normal pulses
- +3 = full pulse or slight increase in pulse volume
- +4 = bounding pulse or increased volume
Veins – neck, arms, legs, etc.
What Is A Normal Pulse Reading
Next: Part II: Assessment Techniques, Con't.
